The Hip Joint
New Hips for Old -- Total Hip Replacement
The surgeon will use your X-rays to assess the amount of damage to the hip, to make measurements, and to form decisions on angles, lengths and drilling depths which must be individualized for each patient. Hip replacement is a form of biological carpentry, which requires careful planning.
Your surgeon will also endeavor to explain to you, as clearly as possible, what you can realistically expect from an artificial hip. Recalling what was said can be difficult, particularly if you have trouble concentrating because of pain. For this reason, it is a good idea to bring along a family member or a close friend to the consultation. It is also important to let your surgeon know about your individual lifestyle so you can be matched with an appropriately designed prosthesis.
Preparing for the Operation
If you decide to have hip replacement surgery, it is important to optimize your health beforehand. Here are some suggestions for doing this:
- If you smoke, try to stop smoking at least three months before surgery. Make an appointment for chest physiotherapy to drain large amounts of mucous from your lungs and open up the air passages.
- Discontinue using aspirin ten days before surgery and other anti-inflammatory drugs seven days before surgery, in order to allow bleeding and clotting times to return to normal.
- Treat anemia, and low serum potassium, if present.
- Have pimples or boils eradicated.
- Have a full medical checkup by your local doctor or specialist physician who may uncover unknown problems that could influence the surgical outcome.
- Have infections treated and cleared up. Infectious organisms anywhere in the body, whether on the skin, in the urinary tract, or sinuses, can travel via the blood to the joint replacement and create problems there.
- Your surgeon may ask you to pre-donate your own blood for your surgery. Three units are usually sufficient for primary surgery and four-five units for revision surgery. Alternatively, you can be matched up with blood from a blood bank donor.
- Your treating surgeon will usually arrange for pathology testing, including blood tests and a urine specimen analysis, X-rays and an electrocardiogram (ECG).
- When the time arrives for surgery, enter hospital with a positive attitude. Recovering your motor skills should be a pleasant experience and the outcome of this experience should improve your life.
On the Day of the Surgery
You will usually be admitted on the day of your surgery. Be sure to take your X-rays with you as they are needed for the operation.
If you are scheduled for hip replacement surgery, your anesthetist will see you beforehand and will discuss the anaesthetic with you. You will be advised as to which anaesthetic will be used. An epidural anaesthetic is local and it may continue to provide pain relief after the surgery is over. Alternatively, if you prefer to sleep through the surgery you may want to ask for a general anaesthetic.
The Operation
Firstly, you will be anaesthetized. If you are likely to have difficulty urinating for awhile, you will be prepared so that the urine can automatically drain out through a tube. You will then be placed securely on your side, cleaned, and covered with sterile drapes for surgery. Antibiotics are usually given intravenously at the beginning of the operation and may be continued for 24 to 48 hours post-operatively. An incision is made in the skin over the upper side of the buttock and certain blood vessels are cauterized to minimize bleeding. Overlying tendons and other tissues are dissected and detached to expose bone and cartilage components of the hip joint.
In order to see the joint clearly, much of the visible fibrous capsule is either removed, or folded back and preserved for later repair. The labrum of the hip socket is also removed so that the head of the femur can be dislocated from the acetabulum. During this dislocation, the ligamentum teres usually tears away from the femoral head.
Next, the diseased head of the femur is sawn off. Osteophytes (abnormal bony growths) are removed from within and around the acetabulum, using a bone chisel.
The cup-shaped acetabulum is reamed out to enlarge its cavity (Fig. 7a). For this, either a hand reamer or a low-speed power tool is used with progressively larger reamers. Enough cartilage is removed to deepen the acetabulum into a hemispherical shape which can hold a metallic acetabular cup that will mate with the head of the artificial femur. Cavities around the cup are filled with bone graft. Sometimes, grafts of ground up bone tissue are also needed to correct defects in the acetabulum.

If using a cemented acetabular cup, several holes may be drilled in the pelvic bone. The cement is injected into the acetabulum and also into the holes of the acetabular cup. The cup is cemented into the acetabulum. Any remaining osteophytes and excess cement are removed. If cementless implants are used, the cup is carefully punched into position and secured there with screws.
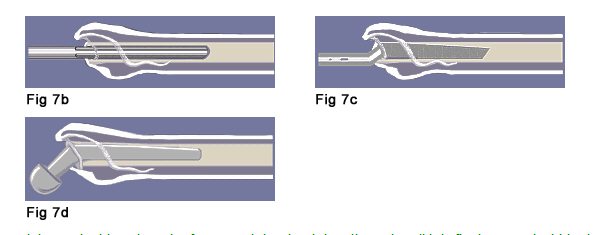
To prepare for the rod-like stem component of the artificial hip, the center of the long axis of the femur must be reamed out. The surgeon starts with the smallest straight reamer and progresses to ones with larger diameters (Fig. 7b). A "broach" (Fig. 7c) is used for the final shaping of the channel. This surgical tool is similar to a rasp file and is shaped like the stem of the trial prosthesis. The final shaping is done in such way that can accommodate the slightly curved and tapered shape of the prosthesis stem (Fig. 7d).
A trial stem is driven into the femur and the depth is adjusted until it is firmly seated within the reamed canal. A hard rubber trial head-neck component is added to the post of the trial stem to determine the correct size to be used. If the neck length appears satisfactory, the hip and leg prosthesis components are temporarily fitted together (reduced). Limb length is reassessed and adjusted. The hip is moved to determine its free range of motion and stability.
Then, the trial prosthesis components are removed and replaced with the final components. Stability is rechecked and, if necessary, the stem is cemented in place. Any debris remaining in the area is removed. The stability of the hip replacement is confirmed and so is its full range of motion. Severed tendons are reattached and the wound is closed.
Surgery for primary hip replacement usually takes one and a half to two hours. Revision surgery or tumor hip surgery can be much longer, depending on the individual hip problem. Revision surgery is highly complex, costly, and requires considerable scientific and technical expertise as well as a supportive health care environment. However, more than 90% of all artificial joints are never revised.
Complications of Hip Surgery
Although many complications may follow total hip replacement, fortunately their incidence is low. Some complications are specifically associated with hip replacement and others can occur with any type of operation that involves anesthesia. Your risk of complications should be discussed pre-operatively with your surgeon.
A. Hip Surgery Complications
- Pain in the thigh groin or knee is usually transient. Chronic (though seldom disabling) thigh pain or groin pain may remain in 2-5% of operated patients.
- Leg length difference of more than 1 cm (less than 1%)
- Limp (2%-5%)
- Nerve injury resulting in pins and needles (less than 1%)
- Nerve injury resulting in foot and leg nerve pain (less than 1%)
- Nerve injury resulting in leg weakness or numbness (about 0.25%)
- A wound infection (0.2%-1%)
- Hip dislocation (4%-10%)
- Thigh bone fracture (2%-5%)
- Excessive bleeding (1%-2%)
B. General Surgery/Anaesthesia Complications
- Nausea and vomiting (transient, mild)
- Cardiac problems, such as heart attack (needs individual, pre-operative assessment)
- Cerebral complications, such as stroke (rare but not 0%)
- Clots blocking blood vessels in the calf (deep venous thrombosis). This can occur with any surgery but is unusually common in hip surgery occurring in 30-50% cases. Most clots are small and asymptomatic and form in the small veins of the leg. In about 1% of cases, this complication is serious.
- Pulmonary embolism (1%)
- Unassociated medical conditions
- Death seldom occurs but it cannot be ruled out (1-2% mortality)
Post-operative Management - Immediate Treatment
Immediately after surgery, a triangle pillow will be placed between your legs to stop your knees from crossing and the thigh on the operated side from bending too far inward. This is changed to an ordinary pillow after two or three days. If no complications occur, you are normally discharged in five-seven days. Stitches or staples are removed at ten days. While in bed, you may be requested to use the pillow for the next four weeks, even after you return home.
Lying or sleeping on the back and on the opposite side is advised. Lying or sleeping on the operated side is not usually permitted for the first six weeks because it increases the risk of dislocation. By the sixth week after surgery, sleeping on the operated side is allowed.
Intravenous antibiotics are usually continued for 24-48 hours postoperatively with timing at the discretion of the operating surgeon. You may also be given anticoagulants to reduce the risk of post-operative clots -- both in the deep veins and the lungs. If you have any new symptom on return home, which is unexplained, consult your doctor or surgeon to deal with it.
Beware! Infection and Delayed Symptoms
It is very important to take infection seriously. If you get any kind of infection, which may show up as fever, pain at the incision site, or swelling of the thigh, see your doctor for infection control immediately. Whenever infection occurs there is a risk that bacteria may travel in the blood stream to the hip replacement and begin to grow around it. This is important to remember, even years after surgery. If the bone containing a hip replacement becomes infected it will most likely have to be removed.
Failure to prevent the spread of bacteria from a simple ear, skin or bladder infection can have a devastating outcome. Some organisms are so difficult to eradicate that a new artificial hip can never be put in for fear of recurrent infection.
If you develop an infection, even years after your hip replacement, ask your medical practitioner to give you antibiotic treatment to protect your hip region. If you require dental work, ask your doctor or dentist for an antibiotic to protect you against infection.
Remember, if any pain or other symptoms in the groin, buttock, thigh or knee belatedly arise from the hip replacement surgery, you should contact your referring doctor or surgeon without delay.
Recovery schedule
For pain and swelling, take an analgesic (painkiller) according to the directions on the box.
Your recovery is highly variable but, in general, you can expect the following recovery schedule:
- At 24-48 hours, sit on a chair
- At 48 hours, walk using a support frame.
- On day 4, graduate to two crutches, climb steps
- At 2-3 weeks, graduate to one crutch
- At 4 weeks, graduate off crutches
- At 4-6 weeks, drive a car and walk any distance (for example, one to two kilometers).
The treating orthopedic surgeon organizes X-rays and follow-up visits to check the hip replacement. It is important for you to be re-examined at regular intervals. This is because complications can develop that you may not recognize.